Achilles Tendon Reconstruction (Noninsertional & Insertional Tendinosis)
Insertional Achilles Calcification Tendonitis - Case
Achilles Tendinosis - MRI
In cases where non-surgical treatment for chronic degeneration of the Achilles tendon has not provided sufficient relief, surgical intervention can be considered. There is an anatomic division of the tendon that determines how we approach surgery. In some patients – the pain and damage to the tendon is approximately 4-6 centimeters above the heel bone – this is termed non-insertional tendinosis. In cases where the pain is more at the level of heel bone – this is termed insertional tendinosis.
Non-insertional tendinosis can be treated with lengthening of the calf muscle (gastrocnemius recession) if there is a contracture of the muscle. The calf muscle, if tight – is lengthened through an incision in the middle of leg, to lengthen the lining (fascia) – not the muscle itself. The reason for considering this procedure – is that there is data that suggests a tight calf muscle is highly associated with Achilles tendon pathology and lengthening of the lining of the muscle has proven to provide relief of the strain on the tendon allowing the body to heal. There is a small risk of weakness associated with this procedure, however – we ensure that the patient has a tight calf muscle on exam and perform this through a small open incision to ensure that we lengthen the fascia and do not injure the muscle to minimize that risk. A small scar and slight loss of the normal calf muscle will occur after this operation. At the same time, in some patients – we will consider injection of concentrated bone marrow aspiration to add mesenchymal signaling cells (“stem cells”) to biologically augment the tendon to improve the change of healing.
If there is no significant evidence of a calf contracture or a calf lengthening does not provide relief, then a debridement of the tendon may be required. This procedure requires an incision along the Achilles tendon, where the damaged tissue is removed and the remaining tendon is sewed back onto itself (tubularized). This surgery does carry a higher risk of scarring and wound complications compared to a calf lengthening, in addition to a longer recovery and is part of the reason why we consider a calf muscle lengthening first in patients who have a contracture. In some cases, the use of amniotic membrane or concentrated bone marrow is used to provide biologic stimulation for healing.
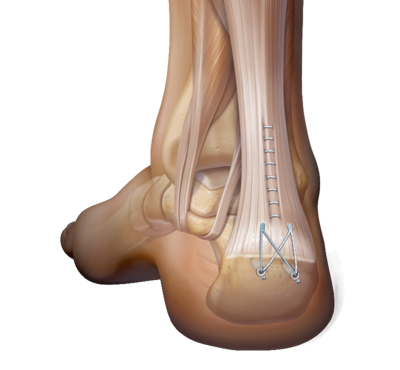
In cases of insertional tendinosis, there is degeneration of the tendon and in many cases – calcification of the tendon as it inserts (attaches) to the back of the heel bone. This is commonly termed a heel spur. In some cases – if the spur is not significantly large, a calf lengthening muscle can be considered. However, if there is a sizeable spur or if the anatomy of the heel bone is part of the problem (in some cases the prominent natural bone is placing pressure on the tendon when the ankle moves up) – then a more aggressive approach is required. In those cases – the tendon is partially detached from the bone and the damaged tendon is removed. The abnormal calcification of the tendon is removed and any prominent bone is removed as well. In many cases, there is sufficient tendon to reconstruct back to the bone and this is performed with a very reproducible technique called the Speedbridge. In cases where the calf is tight – a calf lengthening is done at the same time. Biologic augmentation with amniotic membrane is sometimes considered depending on the extent of the disease. If there is such severe damage to the tendon that only a minimal amount of tendon is viable, the use of a tendon graft or a tendon transfer – where the tendon to the big toe (flexor hallucis longus – FHL) is used to reconstruct the Achilles is required.
Outcomes after Achilles tendon reconstruction:
Decrease in pain - 95% (Reference)
Patient satisfaction - 86% (Reference)
Strength deficit - 13.5-22.3% (Reference), 16.1% (Reference), 30% (Reference), 28-36% (Reference)
Superficial infection - 13% (Reference), 13.3% (Reference), 15.6% (Reference)
Deep would infection - 2.8% (Reference), 6.6% (Reference)
Delayed wound healing - 13% (Reference), 13.8% (Reference)